FOI 24/25-1212
DOCUMENT 1
Specialised driving lessons
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question: 1. How many hours of specialised driving lessons is generally required
for an individual with a disability to learn how to drive and attain their driver’s license? How
does this vary between disability populations (e.g. ABI, Stroke, ID, ASD)?
2. What is the best practice approach for a driver rehabilitation program, are there any
guidelines regarding the frequency of driving lessons and frequency of Driver Trained
Occupational Therapist review/re-assessment?
3. What are the factors which determine successful attainment of licensing, especial y for
individuals with cognitive impairments?
Date: 01/12/2022
Requestor: Melody s47F- personal privacy
Endorsed by: Katrin s47F- personal
privacy
Researcher: Aaron s47F- personal privacy
Cleared by: Stephanie s47F- personal privacy
Review date:
Page 1 of 35
link to page 1 link to page 2 link to page 2 link to page 3 link to page 4 link to page 4 link to page 5 link to page 6 link to page 6
FOI 24/25-1212
1. Contents
Specialised driving lessons ........................................................................................................ 1
1.
Contents ....................................................................................................................... 2
2.
Summary ...................................................................................................................... 2
3.
Guidelines ..................................................................................................................... 3
4.
Evidence for on-road driving lessons ............................................................................ 4
4.1 General ...................................................................................................................... 4
4.2 Autism Spectrum Disorder ......................................................................................... 5
4.3 Traumatic brain injury ................................................................................................ 6
5.
References ................................................................................................................... 6
2. Summary
This paper focussed on on-road driver training interventions for people with cognitive or
emotional concerns which impact their driving. There is very little evidence evaluating on-road
driving lessons despite this being one of the most widespread interventions used for driver
training and rehabilitation. Lack of evidence for on-road driving lessons is a known issue for
researchers and driver trained occupational therapists (DTOTs) and is frequently remarked on
in the research literature.
Relevant studies have been conducted for drivers with Autism Spectrum Disorder (ASD) and
traumatic brain injury (TBI). Surveys of driving instructors suggest learners with ASD may
require 20-40 formal driving lessons. Evidence shows that while most people with TBI can
return to driving, those who require additional training need on average seven 2hr formal
driving lessons. Researchers have explored for other cohorts (stroke, mild cognitive
impairment, psychosocial disability) but available studies were either exploratory (e.g.,
describing driver profiles) or examined other interventions (e.g., simulator training, driver
education, physical rehabilitation etc.).
While there is consistent evidence that suggests people with disability take longer to get their
license, any quantified results are based on very few studies and should be treated with
caution.
No guidelines were found which offered recommendations for duration, frequency or number
of driving lessons for people with cognitive or emotional concerns that might impact their
driving. In response to lack of evidence, guidelines stress the need for individualised
interventions which account for the learners’ specific needs.
Page 2 of 35
FOI 24/25-1212
3. Guidelines
Database searches uncovered no published guidelines recommending an overall approach to
frequency or duration of specialised driving lessons, reviews or reassessments for people with
cognitive or emotional concerns that might impact their driving.
Assessing fitness to drive is a collaboration of AustRoads and the National Transport
Commission and provides guidelines for determining when a driver with some medically
relevant impairment meets licensing requirements (AustRoads & National Transport
Commission, 2022). This includes required frequency of reassessment after a person has
obtained their license. For example, reassessment may be more frequent if a driver has a
progressive condition. However,
Assessing fitness to drive does not provide recommendations
around frequency of reassessment for drivers prior to obtaining their license. Nor does it
provide guidelines around frequency or duration of lessons or rehabilitation strategy for drivers
wanting to gain or regain their license. In fact, the guidelines state explicitly, “there is currently
limited evidence to support the use of particular rehabilitation or retraining strategies”
(AustRoads & National Transport Commission, 2022, p.23).
VicRoad’s
Guidelines for Occupational Therapy Driver Assessors (VicRoads) does include
some recommendations around driving lessons. VicRoads says, for instance, that driving
instructors need to “use appropriate training methods to accommodate the driver’s past
experience, current skil level and communication/impairment needs” (p.33). This might involve
specifying number of lessons or recommending a duration of lessons. However, the guidelines
do not specify how the DTOT’s should recommend frequency or duration of lessons.
Queensland’s
Controlled Environment Driver Training Guidelines (Department of Transport
and Main Roads, 2021) emphasises responding to individual learner circumstances and does
not make recommendations around frequency or duration of lessons:
… consideration should be given to offering flexibility of approach and adapting learning
principles to the needs of individuals, including those students with physical or mental
health challenges. Driver trainers are not expected to conduct clinical assessments of
special needs or challenges, but as educators there is a responsibility to be sensitive to
these issues and to try to respond to them. Unfortunately, there is little research and
evidence to prescribe specific driver training techniques for students with special needs;
however, the key principle is to try to understand their circumstances and be as flexible
in the conduct of training and communication methods as is reasonably practicable
(2021, p.11).
The UK’s
National standard for driver and rider training (National standard, 2020) outlines what
a driver instructor should know when training learner drivers. It describes a client-centred
approach which responds to individual needs and takes into account to prior knowledge and
experience of the learner. It does not provide guidance on frequency or duration of lessons.
Page 3 of 35
FOI 24/25-1212
4. Evidence for on-road driving lessons
There is a notable lack of evidence regarding the efficacy of on-road driving lessons for people
with disabilities. A 2014 systematic review of occupational therapy assisted driver rehabilitation
notes:
while it is our experience that the most common intervention approach used in clinical
practice is a series of lessons with a driving instructor, we were unable to identify any
studies that evaluated this intervention approach. This kind of intervention has received
very limited description in the literature which may be due to the heterogeneous nature
of the training provided. (Unsworth & Baker, 2014, p.112)
While there is some efficacy data published since 2014, the lack of evidence of on-road driving
lessons for people with disabilities is noted in almost all studies referenced in this paper
(AustRoads & National Transport Commission, 2022; Berndt et al, 2022; Vindin et al, 2021;
Department of Transport and Main Roads, 2021; Dun et al, 2020; Sangrar et al, 2019; Wilson
et al, 2018; Lindsay & Stoica, 2018; Unsworth et al, 2015; George et al, 2014). For example,
as recently as 2021, Australian researchers in Perth and Sydney could claim to have
completed the first experimental on-road driving training intervention study for people with ASD
(Vindin et al, 2021, p.3708).
4.1 General
In a recent interview-based study of Australian DTOTs looking at self-reported clinical
reasoning regarding recommendations for interventions, Berndt et al note that:
Participants asserted that peer-reviewed scientific research evidence for particular driver
rehabilitation interventions was sparse, so they often deferred to clinical judgment and
experience to guide practice. In the absence of specific driver rehabilitation intervention
research evidence, general evidence was transferred across to a driver rehabilitation
context, applied and then evaluated (Berndt et al, 2022, p.442).
Unfortunately, the authors do not elaborate on what this general evidence consists of.
Participants reported factors related to on-road driving lessons as crucial to their decision
making. For example, participants noted that in order to determine whether a skil was
acquired, they needed to observe the skil being implemented across multiple lessons, rather
than just once during an assessment. Responses also imply that a DTOT wil create a
hypothesis about the learner’s driving ability and then test the hypothesis over multiple
lessons.
Breault et al (2019) found young learners with disabilities took longer on average to learn to
drive compared to young people without disabilities but did not provide details about average
duration or frequency of lessons.
In their review, Sangrar et al (2019) found interventions including in-vehicle training could
reduce driver errors and improve control of vehicle for older drivers. However, as the
Page 4 of 35
FOI 24/25-1212
interventions generally included multiple components (e.g., simulator training and group
education) it is unclear how much of the effect could be attributed to on-road lessons. Also, the
on-road component of training in these studies was generally limited to one or 2 sessions.
Similar findings for older drivers were reported by Castalucci et al (2020). Beanland and
Huemer (2021) raise the same concern regarding one- or 2-day driver training programs for all
post-license drivers.
4.2 Autism Spectrum Disorder
A 2019 systematic review reported on 3 papers recommending strategies to assist people with
ASD to drive. Strategies included shorter lessons, repetitions of lessons and regular, frequent
and consistent lessons (Lindsay, 2019). The necessity for repeating lessons could be a reason
people with ASD often take longer to learn to drive (Tyler, 2013).
The use of frequent repetition of lessons was supported in two publications reporting on an
interview-based study of driving instructors (Myers et al, 2019; Myers et al, 2021). These
studies always noted other specific strategies around duration and frequency of on-road
driving lessons. One driving instructor suggested a typical pattern was 24hrs formal instruction
from a driving instructor/OT plus another 200 hours of driving practice with parents/carers.
Others described requiring 3 to 4 times more hours of on-road practice for people with ASD
compared to those without. The authors suggested lessons can continue for 2-3 years.
Instructors often recommended a course of driving lessons, followed by months or years of on-
road practice with informal supports. During this time students were instructed to work on
foundational pre-driving skills (e.g., learning to ride a bike or catch public transport
independently) after which they may return for another course of driving lessons.
Participants in the Myers et al study predicted that around 30% of their students eventually got
their license (Myers et al, 2019; Myers et al, 2021). This is consistent with evidence that 1 in 3
young people with ASD acquire their driver’s license (Curry et al, 2018).
In 2018-2019, an Australian team of researchers completed a scoping review and RCT to
examine interventions for young learner drivers with autism (Wilson et al, 2018; Vindin et al,
2021). The scoping review supports the suggestion raised in other studies (Myers et al, 2021;
Myers et al, 2019; Lindsay, 2019; Tyler, 2013) that young drivers with ASD may require more
lessons of shorter duration compared to those without ASD. In a survey of 388 respondents,
Shepard et al (2022) found drivers with ASD typically required 20-40 professional driving
lessons compared to people without who required on average 0-20 lessons, and driver with
ASD typically got their license later. This is consistent with the only other quantified
recommendation of an average of 24 lessons (Myers et al, 2019).
Wilson et al’s (2018) scoping review found interventions reporting simulator or computer-based
training but found no studies examining on-road driving lesson interventions. To address this
gap, the research team designed an RCT to assess the efficacy of an on-road driving program
for 72 young people with ASD (Vindin et al, 2021). In this study, both the intervention and
control group were given 10 driving lessons with driving instructors who were not DTOTs. The
Page 5 of 35
FOI 24/25-1212
intervention group lessons were delivered by instructors trained in an ASD specific driving
program. The control group lessons were delivered by instructors with no additional training.
The researchers found large effect sizes for both groups but found no statistically significant
difference between groups. It is noteworthy that both groups showed significant benefit after a
course of on-road driving lessons with mainstream professional driving instructors. However,
the authors note there is a possibility of self-selection bias resulting in a group of driving
instructors with interest or experience in training young people with ASD.
4.3 Traumatic brain injury
Duration of driver training after traumatic brain injury depends on the severity of the injury
(Schultheis & Whipple, 2014). Estimates for return to driving after TBI range from 42% to 98%.
In their sample of 48 people with traumatic brain injury, Stolwyck et al (2019) found 31 were fit
to drive following an assessment from an occupational therapist, while 9 of the 17 who failed
the assessment were recommended take one or more driving lessons before being
reassessed. Al those who underwent driving lessons were re-assessed and cleared to return
to driving. However, the report does not make clear how many lessons were required for the
cohort of participants who failed the initial test.
Ross et al (2018) found in an Australian sample of 340 people with traumatic brain injury, 72%
passed the initial post-injury driver assessment and of the 28% who failed the initial
assessment, 98% passed after an average of 7 driving lessons (14 specialist driving instructor
hours) and 2.5 on-road assessments (9.8 OT hours and 3.8 specialist driving instructor hours).
Only 7 out of the 340 were not able to return to driving.
5. References
AustRoads & National Transport Commission. (2022).
Assessing fitness to drive for
commercial and private vehicle drivers. Australian Government.
https://austroads.com.au/publications/assessing-fitness-to-drive/ap-g56
Beanland, V and Huemmer, I. (2021)
The effectiveness of advanced driver training. Waka
Kotahi NZ Transport Agency research report 677.
https://nzta.govt.nz/assets/resources/research/reports/677/677-the-effectiveness-of-
advanced-driver-training.pdf
Berndt, A., Hutchinson, C., Tepper, D., & George, S. (2022). Professional reasoning of
occupational therapy driver rehabilitation interventions.
Australian Occupational
Therapy Journal,
69(4), 436–446.
https://doi.org/10.1111/1440-1630.12804
Breault, C., Giroux, L., Gauvreau, A., Belanger, S., Lamontagne, M.-E., & Morales, E. (2019).
Acceptability of the process of obtaining a driver’s license by young people with and
without disabilities.
Journal of Accessibility and Design for Al ,
9(1), 90–117.
https://doi.org/10.17411/jacces.v9i1.198
Page 6 of 35
FOI 24/25-1212
Castellucci, H. I., Bravo, G., Arezes, P. M., & Lavallière, M. (2020). Are interventions effective
at improving driving in older drivers?: A systematic review.
BMC Geriatrics,
20(1), 125.
https://doi.org/10.1186/s12877-020-01512-z
Curry, A. E., Yerys, B. E., Huang, P., & Metzger, K. B. (2018). Longitudinal study of driver
licensing rates among adolescents and young adults with autism spectrum disorder.
Autism: The International Journal of Research and Practice,
22(4), 479–488.
https://doi.org/10.1177/1362361317699586
Department of Transport and Main Roads. (2021). Controlled environment driver training
guidelines. Queensland Government.
https://www.tmr.qld.gov.au/-
/media/busind/accreditations/driverandridertrainers/Controlled-Environment-Driver-
Training-Guidelines.pdf?la=en
Di Stefano, M & Ross, P. (2018).
VicRoads Guidelines for Occupational Therapy Driver
Assessors (3rd edition). Roads Corporation Victoria, Melbourne.
George, S., Crotty, M., Gelinas, I., & Devos, H. (2014). Rehabilitation for improving automobile
driving after stroke.
Cochrane Database of Systematic Reviews,
2, CD008357.
https://doi.org/10.1002/14651858.CD008357.pub2
Myers, R. K., Bonsu, J. M., Carey, M. E., Yerys, B. E., Mol en, C. J., & Curry, A. E. (2019).
Teaching autistic adolescents and young adults to drive: Perspectives of specialized
driving instructors.
Autism in Adulthood Knowledge Practice and Policy,
1(3), 202–209.
https://doi.org/10.1089/aut.2018.0054
Myers, R. K., Carey, M. E., Bonsu, J. M., Yerys, B. E., Mol en, C. J., & Curry, A. E. (2021).
Behind the wheel: Specialized driving instructors’ experiences and strategies for
teaching autistic adolescents to drive.
The American Journal of Occupational Therapy:
Official Publication of the American Occupational Therapy Association,
75(3),
7503180110p1.
https://doi.org/10.5014/ajot.2021.043406
National standard for driver and rider training. (2020). Driver and Vehicle Standards Agency.
https://www.gov.uk/government/publications/national-standard-for-driver-and-rider-
training/national-standard-for-driver-and-rider-training#unit-2---design-learning-
programmes
Lindsay, S. (2017). Systematic review of factors affecting driving and motor vehicle
transportation among people with autism spectrum disorder.
Disability and
Rehabilitation,
39(9), 837–846.
https://doi.org/10.3109/09638288.2016.1161849
Lindsay, S., & Stoica, A. (2017). A systematic review of factors affecting driving and public
transportation among youth and young adults with acquired brain injury.
Brain Injury,
31(10), 1257–1269.
https://doi.org/10.1080/02699052.2017.1321140
Ross, P. E., Di Stefano, M., Charlton, J., Spitz, G., & Ponsford, J. L. (2018). Interventions for
resuming driving after traumatic brain injury.
Disability and Rehabilitation,
40(7), 757–
764.
https://doi.org/10.1080/09638288.2016.1274341
Page 7 of 35
FOI 24/25-1212
Sangrar, R., Mun, J., Cammarata, M., Griffith, L. E., Letts, L., & Vrkljan, B. (2019). Older driver
training programs: A systematic review of evidence aimed at improving behind-the-
wheel performance.
Journal of Safety Research,
71, 295–313.
https://doi.org/10.1016/j.jsr.2019.09.022
Sheppard, E., van Loon, E. & Ropar, D. (2022). Dimensions of Self-Reported Driving Difficulty
in Autistic and Non-Autistic Adults and their Relationship with Autistic Traits.
Journal of
Autism and Developmental Disorders. https://doi.org/10.1007/s10803-021-05420-y
Schultheis, M. T., & Whipple, E. (2014). Driving after traumatic brain injury: evaluation and
rehabilitation interventions.
Current Physical Medicine and Rehabilitation Reports,
2(3),
176–183.
https://doi.org/10.1007/s40141-014-0055-0
Stolwyk, R. J., Charlton, J. L., Ross, P. E., Bédard, M., Marshal , S., Gagnon, S., Gooden, J.
R., & Ponsford, J. L. (2019). Characterizing on-road driving performance in individuals
with traumatic brain injury who pass or fail an on-road driving assessment.
Disability
and Rehabilitation,
41(11), 1313–1320.
https://doi.org/10.1080/09638288.2018.1424955
Tyler S. (2013). Asperger’s syndrome: the implications for driver training methods and road
safety.
Journal of the Australasian College of Road Safety,
24, 55–62.
Unsworth, C. A., & Baker, A. (2014). Driver rehabilitation: a systematic review of the types and
effectiveness of interventions used by occupational therapists to improve on-road
fitness-to-drive.
Accident; Analysis and Prevention,
71, 106–114.
https://doi.org/10.1016/j.aap.2014.04.017
Unsworth, C., Harries, P., & Davies, M. (2015). Using Social Judgment Theory method to
examine how experienced occupational therapy driver assessors use information to
make fitness-to-drive recommendations.
The British Journal of Occupational Therapy,
78(2), 109–120.
https://doi.org/10.1177/0308022614562396
Vindin, P., Cordier, R., Wilson, N. J., & Lee, H. (2021). A driver training program intervention
for student drivers with autism spectrum disorder: A multi-site randomised controlled
trial.
Journal of Autism and Developmental Disorders,
51(10), 3707–3721.
https://doi.org/10.1007/s10803-020-04825-5
Wilson, N. J., Lee, H. C., Vaz, S., Vindin, P., & Cordier, R. (2018). Scoping review of the
driving behaviour of and driver training programs for people on the autism spectrum.
Behavioural Neurology,
2018, 6842306.
https://doi.org/10.1155/2018/6842306
Page 8 of 35
 DOCUMENT
[Research type]
DOCUMENT
[Research type]
FOI 24/25-1212
2
OFFICIAL
For Internal Use Only
Outcome comparison of catheter model and
technique
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question:
Date: 02/03/2022
Requestor: Nicola s47F- personal
privacy
Endorsed by: Charika s47F- personal privacy
Researcher: Aaron s47F- personal privacy
Cleared by: Aaron s47F- personal privacy
1. Contents
Outcome comparison of catheter model and technique ............................................................. 1
1.
Contents ....................................................................................................................... 1
2.
Summary ...................................................................................................................... 2
3.
Catheter types and methods ......................................................................................... 2
4.
Outcomes ..................................................................................................................... 3
4.1 Risk of urinary tract infections .................................................................................... 4
4.2 Other adverse events ................................................................................................ 5
4.3 User preference ......................................................................................................... 5
5.
Cost-effectiveness ........................................................................................................ 5
Catheter comparison
OFFICIAL
Page 9 of 35
 [Research type]
[Research type]
FOI 24/25-1212
OFFICIAL
For Internal Use Only
6.
References ................................................................................................................... 7
2. Summary
Different catheter types and different methods of use, cleaning and management may affect
the comfort, usability and potential risks of catheter use. Due to inconsistency in the literature,
firm conclusions are not possible regarding the effect of different catheter types or methods on
risk of UTI and other health complications. No conclusions can be drawn to suggest
hydrophilic catheters, closed system catheter sets, or ‘no touch’ catheters lower risk of health
complications.
Catheter types and management strategies can vary widely in cost. Reusable non-coated
catheters are the least expensive catheter type by unit cost. The most expensive is likely
single-use, closed-system, hydrophilic catheters. However, when associated costs such as
health-care and employment are included, the overall costs may be different.
Most cost-effectiveness studies from the last 7 years find that hydrophilic catheters are more
cost-effective over a lifetime compared to single-use uncoated catheters. An Australian study
calculates a lifetime saving of $298,450 in favour of hydrophilic catheters. All cost-
effectiveness analyses reviewed are limited by assumptions and inferences that may not be
supported by current evidence. Therefore, it is not possible to say with confidence that the
hydrophilic catheter is more cost-effective than lower cost options.
Risk of urinary tract infection (UTI) and associated health-care costs are a key feature of cost-
effectiveness analyses. Most cost-effectiveness studies fix an incidence rate for UTI for
different types of catheter. The studies finding that hydrophilic catheters are more cost-
effective generally infer a reduced risk of UTI for hydrophilic compared to other types of
catheter. However, this conclusion may not be supported by current evidence.
While there are a number of reviews and meta-analyses which favour hydrophilic catheters for
reducing risk of UTI and other health complications, the evidence is not firm. Several studies
find no difference between catheter types. There is moderate level evidence that hydrophilic
catheters may even increase the risk of urethral trauma.
There are also some notable limitations in the literature. There is significant heterogeneity
especially around the definition of UTI. Studies are often not generalisable due to non-
representative samples and attrition bias.
3. Catheter types and methods
In-dwelling catheterisation involves leaving the catheter in place for a period of time. This is not
the preferred option for most people requiring catheterisation but is still used by around one
third of people with a spinal cord injury (Wu et al, 2022). Intermittent catheterisation involves
Catheter comparison
OFFICIAL
Page 10 of 35
 [Research type]
[Research type]
FOI 24/25-1212
OFFICIAL
For Internal Use Only
inserting and removing a catheter multiple times a day. Catheters used in intermittent
catheterisation may be used once and discarded (single-use) or used multiple times
(reusable). Reusable catheters may be used for one day or for longer periods. They usually
require washing between uses (Wu et al, 2022; Ye et al, 2021; Health Quality Ontario, 2019).
Single-use catheters can be used with either a sterile technique (sterile catheter, gloves, in a
sterile environment as far as possible) or a clean technique (clean hands or gloves). Reusable
catheters can only be used with a clean technique (Prieto et al, 2021; Ye et al, 2021; Health
Quality Ontario, 2019).
Some catheters require the user or carer to add lubricant before insertion. They are referred to
as non-coated catheters to distinguish them from hydrophilic-coated catheters which have a
polymer coating that acts as a lubricant when it interacts with water. Hydrophilic catheters may
also come in sterile packaging with saline solution, which means the user does not need to
add water before insertion. These are called pre-activated hydrophilic catheters. Non-coated
catheters may also come in a sterile package pre-lubricated. Catheters may be purchased by
themselves or with a urine collection bag already attached (Ye et al, 2021; Health Quality
Ontario, 2019).
4. Outcomes
Research on outcomes associated with catheter use focusses on:
incidence of UTIs
other adverse events (like haematuria, urethral trauma, bladder stones etc.)
preference or satisfaction with different types or methods.
Most contemporary research focusses on comparisons of different intermittent catheterisation
techniques using hydrophilic or non-coated catheters. Despite this being a well-researched
area, few firm conclusions are possible. Many systematic reviews and meta-analyses show
inconsistent results.
Due to the quantity of research material available, we have prioritised:
evidence published in the last 7 years (2017-2023)
review articles and cost-effectiveness studies
evidence related to an Australian context where possible.
The following discussion of catheter type and method outcomes is based on 17 systematic
reviews conducted between 2017 and 2023.
Catheter comparison
OFFICIAL
Page 11 of 35
 [Research type]
[Research type]
FOI 24/25-1212
OFFICIAL
For Internal Use Only
4.1 Risk of urinary tract infections
Low level evidence suggests that intermittent catheterisation is associated with fewer UTIs
than in-dwelling catheterisation (Wu et al, 2022; Kinnear et al, 2020).
There is significant disagreement in the literature as to whether hydrophilic catheters are
associated with lower risk of developing a UTI. Some meta-analyses have found a significantly
reduced risk of UTI for people using hydrophilic catheters (Plata et al, 2023; Gauhur et al
2022; Ye et al, 2021; Feng et al, 2020; Rognoni & Taraconi, 2017). However, the results are
not straight-forward. Feng et al (2020) found a 54% reduction in frequency of UTI associated
with use of hydrophilic catheters. Rognoni & Taraconi (2017) found a lower risk of UTI
associated with hydrophilic catheter compared to single-use non-coated catheter. This
contrasts with Plata et al (2023), who found a reduction in frequency of UTIs overall, but not if
the comparison is limited to single-use hydrophilic versus single-use non-coated. They found a
significantly lower risk in adult hydrophilic catheter users but not the paediatric group. Gauhur
et al (2022) found hydrophilic catheters are associated with a statistically significant reduction
in UTIs only if the sub-group is limited to long term catheter users. When comparing all
subjects, there was no significant difference in UTI frequency. Ye et al (2021) found a
significant reduction in UTIs for both hydrophilic and gel-lubricated catheters when compared
to non-coated catheters, but no significant difference between hydrophilic and pre-lubricated
models. There is some low-very low certainty evidence favouring pre-lubricated catheters
presented in other reviews (Health Quality Ontario, 2019; Shamout et al, 2017). A report from
Health Quality Ontario (2019) did not find significantly different levels of risk in the
development of UTI for any catheter type. Prieto et al (2021) note that both higher risk of UTI
and lower risk of UTI are possible considering the margin of error.
This inconsistency is reflected in reviews that did not complete a meta-analysis. Shamout et al
(2017) found only one out of 6 papers reviewed found a significant reduction in risk of UTI
associated with use of hydrophilic catheter. Barken & Vaabengaard (2022) in contrast, found 8
out of 10 studies supported the use of hydrophilic catheters to reduce UTI frequency.
Prieto et al (2021) suggest that the most impactful question regarding risk of UTI is whether
risk is affected by single-use or multiple-use catheter practice. The authors found no
compelling evidence that single- or multiple-use was associated with different rates of UTI.
This is echoed in the Health Quality Ontario report (2019).
Furthermore, there is some emerging evidence that other strategies such as catheter cleaning
techniques or education programs for nurses or carers can decrease risk of UTI for long term
catheter users (Alex et al, 2022; Mitchell et al, 2021; Shamout et al, 2017). However, evidence
is not sufficient to draw a conclusion regarding these interventions (Prieto et al, 2021; Mangal
et al, 2021; Sheperd et al, 2017).
Due to inconsistency of results, firm conclusions are not possible regarding the effect of
different catheter types or methods on risk of UTI. Some limitations are pervasive in the
literature. Reviewers often refer to differences in the definition of UTI to explain the
Catheter comparison
OFFICIAL
Page 12 of 35
 [Research type]
[Research type]
FOI 24/25-1212
OFFICIAL
For Internal Use Only
inconsistency of results (Plata et al, 2023; Barken & Vaabengaard, 2022; Prieto et al, 2021;
Rognoni & Taraconi, 2017). Many studies included in systematic reviews and meta-analyses
have disproportionate levels of male participants and high drop-out rates, especially for
hydrophilic treatment groups (Plata et al, 2023; Ye et al, 2021; Rognoni & Taraconi, 2017).
4.2 Other
adverse
events
Prieto et al (2021) found moderate certainty evidence that non-coated catheters slightly reduce
the risk of urethral trauma and bleeding compared with hydrophilic catheters. Whereas Feng et
al (2020) found a 55% reduction in risk of urethral trauma associated with hydrophilic
catheters. Liao et al (2022) found a significant reduction in microscopic haematuria with
hydrophilic catheters compared to non-coated catheters, but no statistically significant
difference for gross haematuria. Health Quality Ontario (2019) and Plata et al (2023) found a
similar result. Rognoni & Taraconi (2017) found a higher, but non-significant risk of haematuria
for hydrophilic catheters.
4.3 User
preference
Most studies that track user preference favour hydrophilic catheters (Barken & Vaabengaard
2022; Feng et al, 2020; Shamout et al, 2017). Ye et al (2021) found a stronger preference for
pre-activated hydrophilic catheters followed by reusable non-coated, non-preactivated
hydrophilic, pre-lubricated and single-use non-coated. However the differences between these
groups were not significant. Health Quality Ontario (2019) found a stronger preference for pre-
lubricated single use catheters. Prieto et al (2021) found no reliable evidence of difference in
preference between catheter models.
5. Cost-effectiveness
Cost-effectiveness studies have been completed for Australia (Couchman et al, 2022), Japan
(Watanabe et al, 2017), Italy (Rognoni & Tarricone, 2017), United Kingdom (Baker et al, 2023),
Brazil (Truzzi et al, 2018), Canada (Health Quality Ontario, 2019; Welk et al, 2018) and United
States (Hutton et al, 2018). Multiple systematic reviews consider cost-effectiveness of different
catheter models or techniques (Barken & Vaabengaard 2022; Prieto et al 2021; Feng et al
2020; Shamout et al, 2017) but only one was found for which cost-effectiveness was the main
focus (Xi et al, 2021).
Most cost-effectiveness analyses have focussed on costs and outcomes for people with spinal
cord injury (Couchman et al, 2022; Xi et al, 2021; Truzzi et al, 2018; Welk et al, 2018;
Watanabe et al, 2017; Rognoni & Tarricone, 2017). Baker et al (2023) included patients with
either spinal cord injury or multiple sclerosis. Hutton et al (2018) included patients with
indwelling catheters residing in nursing homes. The study from Health Quality Ontario (2019)
focussed on participants with chronic urinary retention.
The international studies from Japan, Canada, UK, USA, Brazil and Italy all suggest that the
single use hydrophilic catheter is a cost-effective option in their respective contexts. This is
Catheter comparison
OFFICIAL
Page 13 of 35
 [Research type]
[Research type]
FOI 24/25-1212
OFFICIAL
For Internal Use Only
primarily due to costs of treatment of UTIs and other complications of UTIs. The exception is
one study from Ontario, Canada, which found multiple-use non-coated catheters were the
most cost-effective option:
Given the marginal differences in total QALYs across catheter types, the lowest-cost
intervention—multiple-use noncoated catheters (one per week)—had the highest
probability of being cost-effective when compared with multiple-use noncoated (one per
day), single-use noncoated, and single-use hydrophilic catheters. Where it may not be
feasible for some patients to clean and reuse catheters, single-use noncoated catheters
have the highest probability of being cost-effective (Health Quality Ontario, 2019, pp.79-
80).
This conclusion likely differs from most other cost-effectiveness analyses due to:
limited horizon of 5 years compared with lifetime horizon of other studies
a very high estimate of the difference in cost between hydrophilic and non-coated
catheters relative to other studies
the authors’ assessment that there is a low level of evidence for significantly
different outcomes for hydrophilic, non-coated catheters and for single or multiple-
use catheters.
Regarding the 5 year horizon, the authors justify this based on limited evidence for the long
term incidence of complications for different catheter types and lack of data on the associated
costs of complications. Other studies either: i) make cost and incidence predictions based on
inferences from related data, or ii) assume costs and risk are constant over a lifetime.
Regarding the high cost estimate, the authors based monthly and unit costs on information
providers made available online. They calculated a minimum of $800 per month for single use
hydrophilic catheters based on a unit cost of $7.02 and a minimum of $135 per month for
single use non-coated catheters based on a unit cost of $1.09 (all prices in Canadian dollars).
In contrast, the other Canadian based cost-effectiveness analysis set prices at $3.77
hydrophilic catheters and $1.07 for non-coated catheters (Welk et al, 2018). The hydrophilic
catheter unit cost is almost double from one study to the next, which is bound to make a
significant difference to the final analysis.
It is important to note that all of these international studies are limited in terms of
generalisability. Conclusions may not transfer to other contexts or service systems. As with the
two Canadian studies, Xi et al (2021) note that the stated difference in costs between
hydrophilic and non-hydrophilic catheters varied considerably between the studies they
reviewed (from $2.49 USD to $24.24 USD per day). Few of the cost-effectiveness studies
reviewed considered other types of catheters, for example, gel-lubricated non-hydrophilic
catheters. All these studies also make assumptions inferences or about the benefits of
hydrophilic catheters which may not be supported by the current evidence. And most
recognise that either important data points are missing or the quality of the included clinical
Catheter comparison
OFFICIAL
Page 14 of 35
 [Research type]
[Research type]
FOI 24/25-1212
OFFICIAL
For Internal Use Only
evidence is low. As such, its not clear if long term costs of either product are under- or over-
estimated.
One study looked at the cost-effectiveness of hydrophilic catheters for people with spinal cord
injury in an Australian context. Couchman et al (2022) found hydrophilic catheters have higher
unit cost, but ultimately provide a more cost-effective option due to reduction in UTIs, quality of
life, life years gained and productivity. Including unit cost and societal costs such as
productivity loss, hospital admissions and treatment for UTIs and other complications, the
authors calculate a lifetime saving of $298,450 in favour of hydrophilic catheters.
This study has some limitations. The authors were not able to source Australian data on UTI
frequency for people with spinal cord injury living in the community or for costs associated with
some UTI complications. They inferred a UTI frequency based on in-hospital incidence and
clinical judgement. Outcomes for hydrophilic catheters (e.g reduction in UTIs) were based on
only meta-analyses which showed a positive effect on UTI frequency in favour of hydrophilic
catheters. A few of those meta-analyses were published over 25 years ago. Furthermore, the
authors note that a longitudinal cost-effective analysis based on real-world cost and health
outcome information would be more reliable.
6. References
Alex, J., Maneze, D., Ramjan, L. M., Ferguson, C., Montayre, J., & Salamonson, Y. (2022).
Effectiveness of nurse-targeted education interventions on clinical outcomes for patients
with indwelling urinary catheters: A systematic review. Nurse education today, 112,
105319. https://doi.org/10.1016/j.nedt.2022.105319
Baker, H., Avey, B., Overbeck Rethmeier, L., Mealing, S., Lynge Buchter, M., Averbeck, M. A.,
& Thiruchelvam, N. (2023). Cost-effectiveness analysis of hydrophilic-coated catheters
in long-term intermittent catheter users in the UK. Current medical research and
opinion, 39(2), 319–328. https://doi.org/10.1080/03007995.2022.2151734
Barken, K. B., & Vaabengaard, R. (2022). A scoping review on the impact of hydrophilic versus
non-hydrophilic intermittent catheters on UTI, QoL, satisfaction, preference, and other
outcomes in neurogenic and non-neurogenic patients suffering from urinary
retention. BMC urology, 22(1), 153. https://doi.org/10.1186/s12894-022-01102-8
Feng, D., Cheng, L., Bai, Y., Yang, Y., & Han, P. (2020). Outcomes comparison of hydrophilic
and non-hydrophilic catheters for patients with intermittent catheterization: An updated
meta-analysis. Asian journal of surgery, 43(5), 633–635.
https://doi.org/10.1016/j.asjsur.2019.12.009
Gauhar, V., Castellani, D., Teoh, J. Y., Nedbal, C., Chiacchio, G., Gabrielson, A. T., Heldwein,
F. L., Wroclawski, M. L., de la Rosette, J., Donalisio da Silva, R., Galosi, A. B., &
Somani, B. K. (2022). Catheter-Associated Urinary Infections and Consequences of
Using Coated versus Non-Coated Urethral Catheters-Outcomes of a Systematic
Catheter comparison
OFFICIAL
Page 15 of 35
 [Research type]
[Research type]
FOI 24/25-1212
OFFICIAL
For Internal Use Only
Review and Meta-Analysis of Randomized Trials. Journal of clinical medicine, 11(15),
4463. https://doi.org/10.3390/jcm11154463
Health Quality Ontario (2019). Intermittent Catheters for Chronic Urinary Retention: A Health
Technology Assessment. Ontario health technology assessment series, 19(1), 1–153.
Hutton, D. W., Krein, S. L., Saint, S., Graves, N., Kolli, A., Lynem, R., & Mody, L. (2018).
Economic Evaluation of a Catheter-Associated Urinary Tract Infection Prevention
Program in Nursing Homes. Journal of the American Geriatrics Society, 66(4), 742–747.
https://doi.org/10.1111/jgs.15316
Kinnear, N., Barnett, D., O'Callaghan, M., Horsell, K., Gani, J., & Hennessey, D. (2020). The
impact of catheter-based bladder drainage method on urinary tract infection risk in
spinal cord injury and neurogenic bladder: A systematic review. Neurourology and
urodynamics, 39(2), 854–862. https://doi.org/10.1002/nau.24253
Liao, X., Liu, Y., Liang, S., & Li, K. (2022). Effects of hydrophilic coated catheters on urethral
trauma, microtrauma and adverse events with intermittent catheterization in patients
with bladder dysfunction: a systematic review and meta-analysis. International urology
and nephrology, 54(7), 1461–1470. https://doi.org/10.1007/s11255-022-03172-x
Mangal, S., Pho, A., Arcia, A., & Carter, E. (2021). Patient and Family Engagement in
Catheter-Associated Urinary Tract Infection (CAUTI) Prevention: A Systematic
Review. Joint Commission journal on quality and patient safety, 47(9), 591–603.
https://doi.org/10.1016/j.jcjq.2021.05.009
Mitchell, B., Curryer, C., Holliday, E., Rickard, C. M., & Fasugba, O. (2021). Effectiveness of
meatal cleaning in the prevention of catheter-associated urinary tract infections and
bacteriuria: an updated systematic review and meta-analysis. BMJ open, 11(6),
e046817. https://doi.org/10.1136/bmjopen-2020-046817
Plata, M., Santander, J., Zuluaga, L., Torres-Sandoval, C., Valencia, S., Azuero, J., & Trujillo,
C. G. (2023). Hydrophilic versus non-hydrophilic catheters for clean intermittent
catheterization: a meta-analysis to determine their capacity in reducing urinary tract
infections. World journal of urology, 41(2), 491–499. https://doi.org/10.1007/s00345-022-
04235-5
Prieto JA, Murphy CL, Stewart F, Fader M. Intermittent catheter techniques, strategies and
designs for managing long-term bladder conditions. Cochrane Database of Systematic
Reviews 2021, Issue 10. Art. No.: CD006008. DOI:
10.1002/14651858.CD006008.pub5. Accessed 27 February 2023
Rognoni, C., & Tarricone, R. (2017a). Intermittent catheterisation with hydrophilic and non-
hydrophilic urinary catheters: systematic literature review and meta-analyses. BMC
urology, 17(1), 4. https://doi.org/10.1186/s12894-016-0191-1
Catheter comparison
OFFICIAL
Page 16 of 35
 [Research type]
[Research type]
FOI 24/25-1212
OFFICIAL
For Internal Use Only
Rognoni, C., & Tarricone, R. (2017b). Healthcare resource consumption for intermittent urinary
catheterisation: cost-effectiveness of hydrophilic catheters and budget impact
analyses. BMJ open, 7(1), e012360. https://doi.org/10.1136/bmjopen-2016-012360
Shamout, S., Biardeau, X., Corcos, J., & Campeau, L. (2017). Outcome comparison of
different approaches to self-intermittent catheterization in neurogenic patients: a
systematic review. Spinal cord, 55(7), 629–643. https://doi.org/10.1038/sc.2016.192
Shepherd AJ, Mackay WG, Hagen S. Washout policies in long-term indwelling urinary
catheterisation in adults. Cochrane Database of Systematic Reviews 2017, Issue 3. Art.
No.: CD004012. DOI: 10.1002/14651858.CD004012.pub5. Accessed 28 February 2023
Truzzi, J. C., Teich, V., & Pepe, C. (2018). Can hydrophilic coated catheters be beneficial for
the public healthcare system in Brazil? - A cost-effectiveness analysis in patients with
spinal cord injuries. International braz j urol : official journal of the Brazilian Society of
Urology, 44(1), 121–131. https://doi.org/10.1590/S1677-5538.IBJU.2017.0221
Xi, M., Elterman, D. S., Welk, B., Pakosh, M., & Chan, B. C. F. (2020). Cost-effectiveness of
hydrophilic-coated urinary catheters for individuals with spinal cord injury: A systematic
review. BJUI compass, 2(2), 71–81. https://doi.org/10.1002/bco2.63
Watanabe, T., Yamamoto, S., Gotoh, M., Saitoh, T., Yokoyama, O., Murata, T., & Takeda, M.
(2017). Cost-Effectiveness Analysis of Long-Term Intermittent Self-Catheterization with
Hydrophilic-Coated and Uncoated Catheters in Patients with Spinal Cord Injury in
Japan. Lower urinary tract symptoms, 9(3), 142–150. https://doi.org/10.1111/luts.12122
Welk, B., Isaranuwatchai, W., Krassioukov, A., Husted Torp, L., & Elterman, D. (2018). Cost-
effectiveness of hydrophilic-coated intermittent catheters compared with uncoated
catheters in Canada: a public payer perspective. Journal of medical economics, 21(7),
639–648. https://doi.org/10.1080/13696998.2018.1443112
Wu, S. Y., Jhang, J. F., Liu, H. H., Chen, J. T., Li, J. R., Chiu, B., Chen, S. L., & Kuo, H. C.
(2022). Long-Term Surveillance and Management of Urological Complications in
Chronic Spinal Cord-Injured Patients. Journal of clinical medicine, 11(24), 7307.
https://doi.org/10.3390/jcm11247307
Catheter comparison
OFFICIAL
Page 17 of 35
link to page 18 link to page 18 link to page 19 link to page 19 link to page 19 link to page 20 link to page 20
FOI 24/25-1212
DOCUMENT 3
Project management and quality tools
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question: Are there existing project management tools that integrate quality assurance tools or quality
frameworks?
What are the benefits or drawbacks of different project management and quality tools and in
what contexts are they applicable?
Date: 21/11/2023
Requestor: Fiona s47F- personal privacy
Endorsed by: n/a
Researcher: Aaron s47F- personal privacy
Cleared by: Stephanie s47F- personal privacy
1. Contents
Project management and quality tools ....................................................................................... 1
1.
Contents ....................................................................................................................... 1
2.
Summary ...................................................................................................................... 2
3.
NDIA ............................................................................................................................. 2
4.
Australian Public Service .............................................................................................. 2
5.
Quality frameworks ....................................................................................................... 3
6.
References ................................................................................................................... 3
Page 18 of 35
FOI 24/25-1212
2. Summary
NDIA and other Australian Public Services provide helpful quality tools as part of their project
management processes.
Many health and human services have developed quality frameworks which may be modified
to apply in an NDIA context.
3. NDIA
NDIA’s Delivery and Change Office has provided quality tools in the context of their
Project
Delivery Framework Toolkit. The Project Status Report can assist in monitoring the progress of the project, keeping track of
risks and benefits.
A Benefits Score Card is integrated into t
he Project Management and Change Plan as well as
t
he Project Delivery Framework Toolkit. This is a way of specifying how the benefits of a
project wil be measured and monitoring whether the benefits are being achieved according to
the prespecified measures.
4. Australian Public Service
The Australian Public Service Commission (APSC, 2021a) recognises two approaches to
project management: traditional and Agile. Both are aimed to maintain quality of output.
To facilitate the traditional approach, APSC provides
a workplan template and suggests use of
tools such as Gannt charts. This can work well when the project requires a steady methodical
approach:
Traditional project management approaches can provide a greater degree of confidence
in the final deliverable, as the entire project is planned upfront with limited scope for
changing requirements; the downside is that later stages can’t begin until those
preceding it are completed, which can make it difficult to rectify issues if they arise, or if
the direction of the project needs to change (APSC, 2021b).
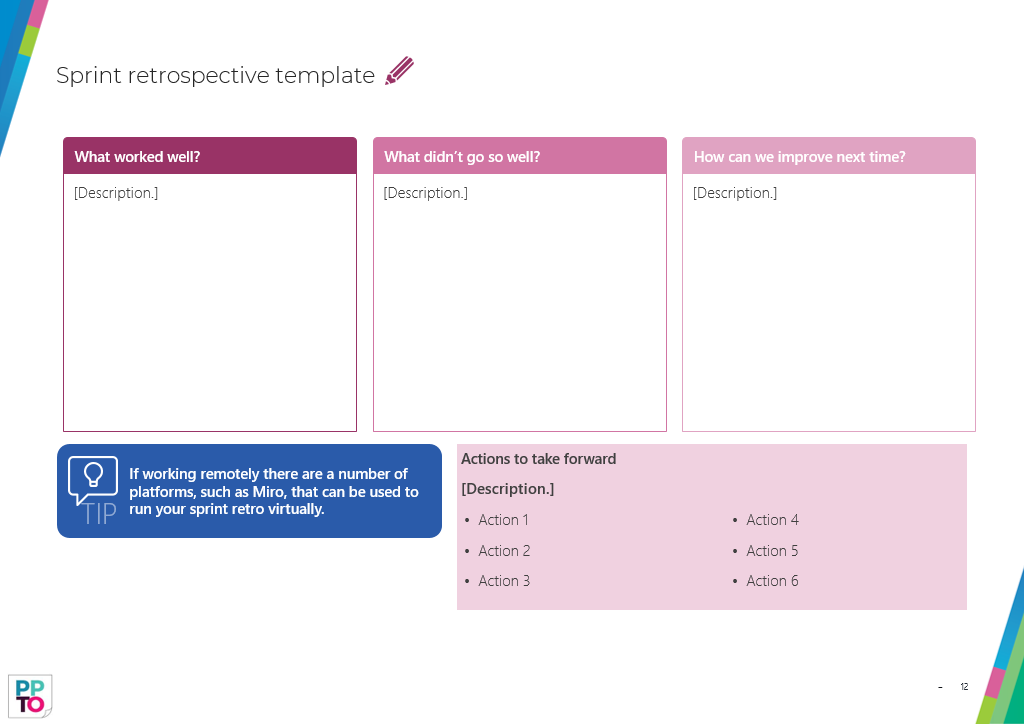
To facilitate the Agile approach, APSC suggests use of the Department of Prime Minister and
Cabinet’s
Agile policy playbook. Agile projects can include use of generic tools such as
Kanban boards, or frequent reflective processes (refer to
Figure 1). This can work when the
project make require multiple changes and revisions based on contextual or stakeholder
changes: “Agile is an iterative project management approach which drives process by working
on ideas and products early and testing and refining them to increase value and impact of the
final product” (APSC, 2021b).
APSC recommends
evaluation tools to complete after the conclusion of a project to provide an
opportunity for quality improvement. This can be similar to
Figure 1. For example, considering
Page 19 of 35
FOI 24/25-1212
whether the project met the taskforce scope or objectives, you can ask “What went well?”,
“What didn’t go well?”, “What are the lessons learned?” (APSC, 2021c).
Figure 1 Sprint retrospective template (Source: Department of Prime Minister and
Cabinet, 2020)
5. Quality frameworks
• NDIA’s National Access and Review branch published their
Quality Framework.
• NDIA’s Complaints branch has published their
Complaints Quality Framework and
Checklist.
• Victorian Government’s Health and Human Services
Community services quality
governance framework.
• Queensland Government’s Department of Communities, Child Safety and Disability
Service
s Human Services Quality Framework. They also include a number of
tools
and resources for implementation of the Framework.
• Australian Commission on Safety and Quality in Healthcare has publis
hed a report
on developing t
he National Safety and Quality Framework for Australia.
6. References
Page 20 of 35
FOI 24/25-1212
Australian Public Service Commission (2021a).
Develop a workplan. Australian Government.
https://www.apsc.gov.au/initiatives-and-programs/workforce-information/taskforce-
toolkit/project-management/develop-workplan
Australian Public Service Commission (2021b).
Effective project management. Australian
Government.
https://www.apsc.gov.au/initiatives-and-programs/workforce-
information/taskforce-toolkit/project-management/effective-project-management
Australian Public Service Commission (2021c ).
Closing down and lessons learned. Australian
Government.
https://www.apsc.gov.au/node/391
Department of Prime Minister and Cabinet. (2020). Agile policy playbook. Australian
Government.
https://www.apsc.gov.au/sites/default/files/2021-
03/agile_policy_playbook.pptx
Page 21 of 35
DOCUMENT 4
FOI 24/25-1212
Physiotherapy and exercise for progressive
neurological conditions
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research questions: What is considered best practice for the frequency and duration of physiotherapy and
exercise physiology for progressive neurological conditions?
Are there any contraindications for use of a delegated care model for these supports with
this population (e.g. using therapy assistants)?
What are the risks and contraindications of physiotherapy and exercise physiology based on
disease progression with these populations (i.e. is there a time when hands on therapy
should not be provided as risks outweigh benefits)?
Date: 29/4/2024
Requestor: s47F - personal privacy
Endorsed by: Shannon As47F - persona
Researcher: Aaron Hs47F - personal priva
Cleared by: Aaron Hs47F - personal priva
Page 22 of 35
FOI 24/25-1212
1. Contents
Physiotherapy and Exercise physiology for progressive neurological conditions ....................... 1
1.
Contents ....................................................................................................................... 2
2.
Summary ...................................................................................................................... 3
3.
Previous TAPIB research .............................................................................................. 3
4.
Therapy assistants ........................................................................................................ 4
5.
Amyotrophic lateral sclerosis / motor neuron disease ................................................... 5
5.1 Frequency and duration ............................................................................................. 5
5.2 Risks .......................................................................................................................... 5
5.3 Stage of progression .................................................................................................. 5
6.
Parkinson’s Disease ..................................................................................................... 6
6.1 Frequency and duration ............................................................................................. 6
6.2 Risks .......................................................................................................................... 7
6.3 Stage of progression .................................................................................................. 8
7.
Multiple Sclerosis .......................................................................................................... 8
7.1 Frequency and duration ............................................................................................. 8
7.2 Risks .......................................................................................................................... 9
7.3 Stage of progression ................................................................................................ 10
8.
Muscular dystrophy ..................................................................................................... 10
8.1 Frequency and duration ........................................................................................... 10
8.2 Risks ........................................................................................................................ 11
8.3 Stage of progression ................................................................................................ 11
9.
References ................................................................................................................. 11
Page 23 of 35
FOI 24/25-1212
2. Summary
This paper considers the use of physiotherapy and exercise interventions for people with
progressive neurological conditions including amyotrophic lateral sclerosis (ALS) and motor
neuron disease (MND), Parkinson’s disease (PD), multiple sclerosis (MS), and muscular
dystrophy (MD). This paper focusses on evidence of optimal frequency and duration of
physiotherapy and exercise interventions, risks associated with interventions, differing care for
early or late stages of progression and the use of therapy assistants through a delegated care
model.
No studies were found that address the role of therapy assistants in the delivery of
physiotherapy or exercise interventions for people with progressive neurological conditions.
Some evidence suggests that the use of therapy assistants in acute hospital settings and
general community settings is safe and effective. This evidence is uncertain and further
research is required.
There is limited evidence regarding optimal dosage of physiotherapy and exercise
interventions for people with progressive neurological conditions. Clinical practice guidelines
for PD and MS provided recommendations for frequency and duration of physiotherapy and
exercise interventions. However, it is likely that these recommendations are based primarily on
clinical judgement rather than published evidence. One 2023 systematic review was able to
determine that at least twice weekly sessions of more than 40 minutes is an effective dose of
exercise intervention for the improvement of balance in MS (Corrini et al, 2023). No other
studies could provide evidence-based dosage recommendations.
Where evidence is not clear, guidelines generally recommend that type, frequency, duration
and intensity of physiotherapy or exercise interventions should be determined individually
based on the needs and preferences of the person receiving treatment.
Despite some issues with the proper reporting of adverse events in experimental studies,
exercise interventions for people with progressive neurological conditions are generally
believed to be safe, provided that standard safety precautions are observed.
There is little evidence regarding safety and effectiveness of physiotherapy and exercise
interventions for people at late stages of progressive neurological conditions. Most research
focusses on people with mild to moderate symptom severity.
3. Previous TAPIB research
Other relevant TAPIB research papers include:
• RES 322 Manual therapy to address neuromusculoskeletal function
• RES 321 Osteopathy
• RES 318 Exercise physiology and stroke
• RES 289 Lokomat Therapy
Page 24 of 35
FOI 24/25-1212
• RES 264 Chiropractic
• RES 233 Virtual reality as a support tool
• RES 191 Massage Therapy as a Treatment for Multiple Sclerosis
4. Therapy assistants
Therapy assistants are
support staff who complete clinical and non-clinical tasks under the supervision and
delegation of an allied health professional. Clinical tasks include any direct therapeutic
interventions provided to patients such as exercise therapy and education, while non-
clinical tasks may include administration duties (eg, completing paperwork for
equipment hire), maintenance of equipment and cleaning the clinical environment.
Because al ied health assistants cannot perform clinical tasks that involve diagnosing or
assessing patient health conditions, allied health professionals must perform a
comprehensive assessment of the patient and prescribe appropriate therapy prior to
delegating the allied health assistant to perform any clinical tasks. (Snowdon et al, 2024,
p.2).
In a survey of 232 UK-based physiotherapists, 81% of respondents indicated that they at least
sometimes delegate the supervision of prescribed exercises to therapy assistants
(Sarigiovannis et al, 2022). The authors also found that delegation of clinical tasks to therapy
assistants was more likely in less complex cases where there is a straightforward treatment
plan. There is a perception that increased reliance on therapy assistants may compromise the
quality or safety of the intervention (Snowdon et al, 2024). However, existing evidence
suggests that physiotherapy or exercise interventions delivered by a therapy assistant are
likely safe (Lau et al, 2024; Snowdon et al, 2020).
No studies were found that address the role of therapy assistants in the delivery of
physiotherapy or exercise interventions for people with progressive neurological conditions.
Where there is minimal research to date, there is a growing interest in the role of therapy
assistants in completing clinical physiotherapy tasks (Snowdon et al, 2024; Sarigiovannis et al,
2023). Current research mostly considers the addition of therapy assistants to usual care
rather than a model where physiotherapy or exercise interventions are primarily delivered by a
therapy assistant (Snowdon et al, 2024; Lau et al, 2024; Snowdon et al, 2020). Some evidence
points to the efficacy and safety of physiotherapy or exercise interventions delivered by
therapy assistants. Additional supervised exercise sessions may improve outcomes regardless
of whether it is delivered by a physiotherapist or therapy assistant (Snowdon et al, 2024; Lau
et al, 2024; Baumann et al, 2023a-b; Sarigiovannis et al, 2023; Sarigiovannis et al, 2022;
Sarigiovannis et al, 2021). Much of the research is based in a hospital setting and the roles of
physiotherapist and therapy assistant are frequently poorly reported, so results may not
generalise across all models of therapy assistance or patient cohorts (Sarigiovannis et al,
2021; Snowdon et al, 2020).
Page 25 of 35
FOI 24/25-1212
5. Amyotrophic lateral sclerosis / motor neuron disease
5.1 Frequency and duration
We did not find any reviews able to determine optimal frequency or duration of exercise or
physiotherapy interventions for people with ALS/MND. One review (Zhou et al, 2022) showed
inconsistent evidence that more intensive exercise training could slow the decline in functional
capacity. However, the authors do not specify what they mean by ‘intensive’.
A 2023 meta-analysis including 17 studies was unable to determine optimal exercise dosage
due to the variability of intervention: “frequency ranged from 2×/week to 3×/day, up to 7
days/week, with repetitions of sets ranging from 20 to 25, intensity ranging from 30 to 60% of a
patient’s maximum value, and treatment duration ranging from 2 weeks to 2 years” (Donohue
et al, 2023, p.19). Meng et al (2020) and Papadopolou et al (2024) were similarly unable to
determine the most effective frequency, intensity, type, timing or duration of exercise-based
interventions.
5.2 Risks
Researchers report some reluctance to prescribe exercise for people with ALS/MND due to
possibility that exercise might lead to fatigue and faster progression of symptoms (MND
Australia, 2021). However, recent reviews have found no serious adverse events in studies of
exercise or physiotherapy intervention for people with ALS/MND (Papadopolou et al, 2024;
Donohue et al, 2023; Meng et al, 2020). Researchers suggest that physiotherapy or exercise-
based interventions are likely safe for people with ALS/MND.
5.3 Stage of progression
Minimal evidence is available for the efficacy of physiotherapy or exercise programs for people
with more advanced ALS/MND. Donahue et al (2023) find some low certainty evidence that
exercise programs are beneficial in early stages of disease progression. However, all of the
studies included in their review explore exercise intervention only on those with low to
moderate symptom severity.
Ireland’s
Guidelines for the physiotherapy management of Motor Neuron Disease (O’Callaghan, 2014), suggests physiotherapy treatment plans differentiate early, middle and
late stages of progression. During the late stage, strategies to maintain function and manage
symptoms may include:
• a stretching program
• active and passive range of movement exercises
• the use of assistive technology such as motomed or tilt table.
Page 26 of 35
FOI 24/25-1212
While evidence is presented for the efficacy of exercise at the early stages of MND,
recommendations for strategies at the middle and late stages are based on clinical judgment
of the authors.
6. Parkinson’s Disease
6.1 Frequency and duration
There is no consensus on optimal frequency or duration of physiotherapy or exercise
interventions for people with Parkinson’s disease. Reviews report average frequency and
duration of interventions used in studies but are unable to determine best practice timing
(Ernst et al, 2024; El Hayek et al, 2023; Osborne et al, 2022; Grimes et al, 2019; NICE, 2017;
Keus et al, 2014).
El Hayek et al (2023) reviewed 46 studies to determine most effective types, timing, frequency,
duration, and outcomes of physiotherapy and exercise for people with Parkinson’s disease.
They found no significant difference between interventions and comparisons for frequency,
duration or number of sessions.
A 2024 Cochrane review of studies on exercise intervention for people with Parkinson’s
disease was unable to draw conclusions regarding the optimal frequency of exercise
intervention (Ernst et al ,2024). The authors observed a beneficial effect on functional mobility
and balance in studies lasting longer than 12 weeks. However, they did not observe a
significant effect of intervention duration on other outcomes.
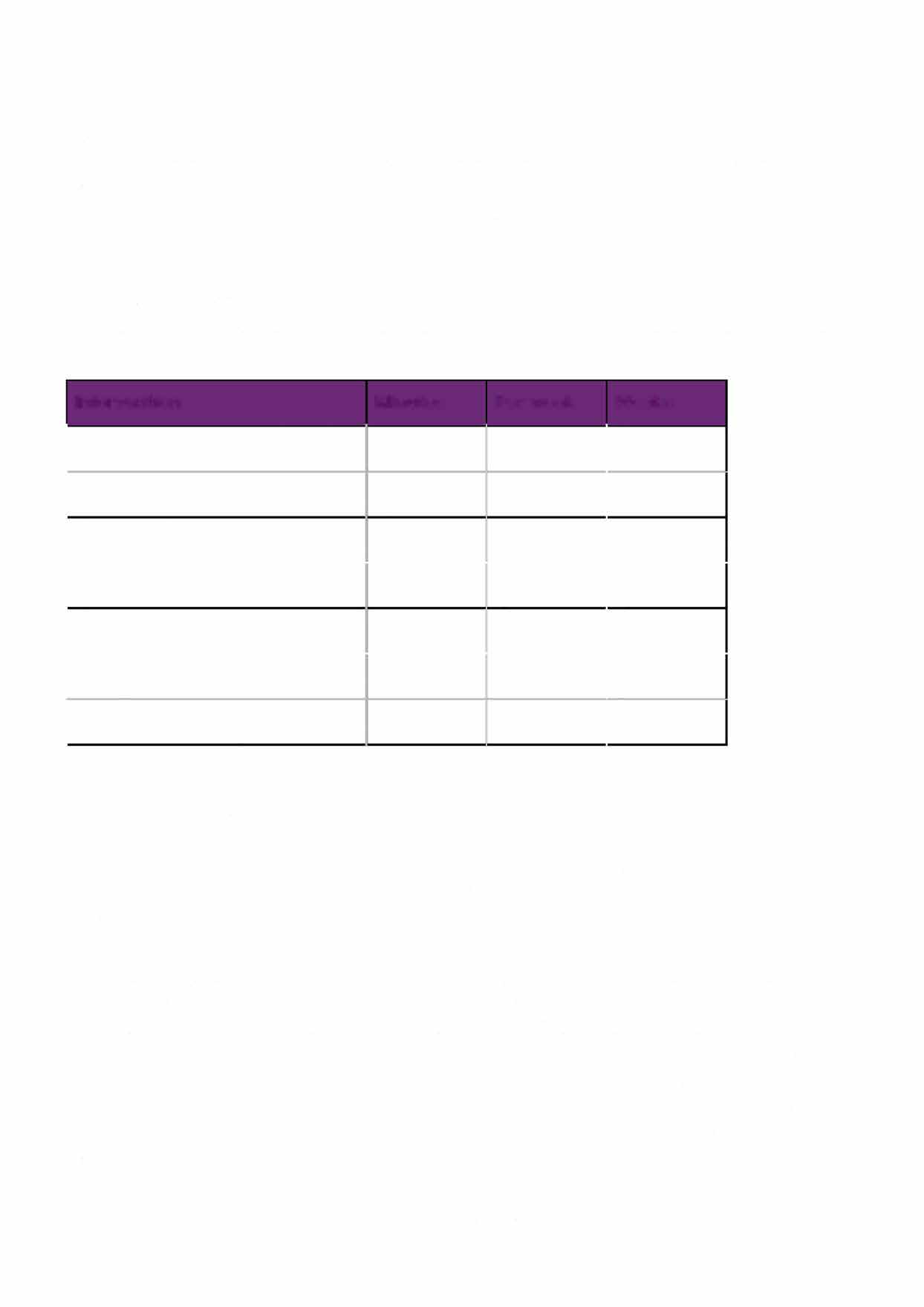
Of four clinical practice guidelines that recommend the use of physiotherapy, exercise or
physical activity for people with Parkinson’s disease, only one provides recommendations
regarding frequency and duration of activity (Osborne et al, 2022; Grimes et al, 2019; NICE,
2017; Keus et al, 2014). The
European Physiotherapy Guideline for Parkinson’s Disease (Keus et al, 2014) includes recommendations for minimum treatment period for seven
physiotherapy modalities (refer to Table 1). However, the Guideline Development Group
(GDG) responsible for the recommendations also note:
Evidence-based information on the optimal number of sessions a week, session time
and length of a treatment period are unavailable. These decisions wil depend on the
treatment goal, the selected intervention, the potential of the [person with Parkinson’s
disease] and the response to the treatment. GDG recommendations for minimum
treatment period, frequency and session duration for each intervention category
provided in this chapter are based on the averages of controlled clinical trials (CCTs)
supportive to the ‘for’ recommendations (Keus et al, 2014, p.64)
Further, the GDG suggests that the optimal treatment period, duration and intensity will most
likely never be determined due to the varied fitness levels, functional capacity and preferences
of people with Parkinson’s disease (Keus et al, 2014, p.72). This judgement is implicitly
supported by the most recent clinical guideline from the American Physical Therapy
Page 6 of14
Page 6 of 14
Page 27 of 35
 Research
Research
FOI
paper
24/25-1212
OFFICIAL
For Internal Use Only
Association (Osborne et al, 2022). Osborne et al review 11 physiotherapy interventions and
concludes there is still insufficient evidence to determine optimal dosing for any of the
reviewed interventions.
Table 1 Minimum recommended treatment period for physiotherapy interventions
(source: Keus et al, 2014)
Note: This table contains recommended minimum treatment periods from the
European
Physiotherapy Guideline for Parkinson's Disease. These recommendations are not the optimal
dosage, but rather the average treatment period of studies that found beneficial effects of the
intervention.
Intervention
Minutes
Per week
Weeks
Conventional physiotherapy
45
3
8
Treadmill training
30
3
4
Dance
60
2
10
Tai chi
60
2
24
Trigger point massage
45
2
8
Cueing
30
3
3
Complex motor sequences
30
3
3
6.2 Risks
Ernst et al (2024) reviewed 154 controlled studies of exercise interventions for people with
Parkinson's disease. They found only 85 studies reported on presence or absence of adverse
events. Falls were reported in 18 studies and pain in 10 studies. The authors note "although
our review pointed out the difficulties in synthesizing the evidence on the comparative safety of
different types of physical exercise, our results are consistent with previous research
suggesting that, in general, physical exercise seems to be relatively safe" (p.64)
Osborne et al (2022) reviewed risks reported in studies of aerobic exercise, resistance training,
balance training, flexibility training, external cueing, community-based exercise, gait training,
task specific training, and a behaviour change approach. They note that there is minor risk if
standard safety procedures are in place. People prescribed exercise should be screened for
heart issues or other health concerns that would preclude moderate to high intensity exercise.
If intensity and duration of exercise is increased, it should be done gradually to prevent injury.
Minor musculoskeletal injuries were reported in studies of aerobic exercise, but these
resolved. Falls and other adverse effects were reported in some studies, though no study
Physic and exercise for progressive conditions
OFFICIAL
Page 28 of 35
FOI 24/25-1212
reported a more significant rate of adverse effects in the intervention group compared to the
control group.
6.3 Stage of progression
Li et al (2023) suggest that exercise interventions are beneficial for people at advanced stages
of Parkinson’s disease to maintain function and health. However, this suggestion was not
based on the results of their review, which found no evidence that exercise could limit
progression of symptoms for people at advanced stages.
Other reviews have also been unable to determine whether exercise interventions are effective
or safe for people at advanced at stages of Parkinson’s progression (stages 4 or 5 of the
Hoehn & Yahr scale). Ernst et al (2024) reviewed 154 studies and found most studies included
participants at stages 1 – 3. No studies included participants at stage 5, while only 17 studies
included participants at stage 4. Therefore, the authors note that their results may not apply to
people at advanced stages of Parkinson’s disease progression.
For most physiotherapy interventions reviewed by Osborne et al (2022), studies supporting the
intervention focussed on mostly those with mild to moderate symptoms covering Hoehn &
Yahr stages 1 to 3. Studies investigating external cueing and resistance, balance and flexibility
training included participants at stages 1 to 4. None of the recommendations made by
Osborne et al are relevant to people showing advanced stage 5 symptoms.
7. Multiple Sclerosis
7.1 Frequency and duration
A 2019 systematic review of clinical practice guidelines for exercise interventions for people
with Multiple Sclerosis found consistent dosage recommendations for aerobic and resistance
training:
The literature we summarized consistently indicated that moderate-intensity aerobic
training should be performed 2 to 3 days per week in 10- to 40-minute bouts. By
achieving these guidelines, people with MS can potentially improve their cardiovascular
fitness, mobility and symptoms of fatigue and depression. This should be complemented
by 2 to 3 days of weekly resistance training, from which anticipated benefits could
include: improved strength, balance, mobility, performance of activities of daily living,
and symptoms of fatigue (Kim et al, 2019, p.9).
These recommendations may be based on a combination of experimental evidence and
clinical judgement. However, considering the difficulty of deriving optimal dosage levels from
the current evidence, it is likely that the recommendations in Kim et al represent a professional
consensus rather than an evidence-based conclusion (Taul-Madsen et al, 2021; Edwards &
Pilutti, 2017).
Page 29 of 35
FOI 24/25-1212
Corrini et al (2023) reviewed 20 randomised controlled trials looking at the effect of balance
training programs for people with Multiple Sclerosis. They found high quality evidence that
physiotherapy targeting balance has a moderate effect on improving balance as measured by
the Berg Balance Scale. In addition, their meta-analysis was able to show that sessions lasting
40 minutes or longer produced a significant and clinically meaningful improvement in balance
scores, while sessions lasting under 40 minutes did not produce statistically significant results.
The authors concluded that:
intense treatments lasting at least 40 [minutes] were associated with a better and more
clinically meaningful improvement, and greater results can be reached when
rehabilitation is provided over a short period (duration) and for a few sessions per week
(frequency) (Corrini et al, 2023, p.20).
7.2 Risks
Learmonth et al (2023) searched for information on relapse and adverse events after exercise
interventions for people with Multiple Sclerosis. They reviewed 40 randomised controlled trials
including 1780 participants. The authors found no significant difference in adverse events
between exercise intervention and comparison groups. The analysis
did not reveal any significant variability in risk of exercise training across the potentially
important factors of exercise type, delivery style (e.g. supervised, independent or
remotely supervised), participant disability level or the prescription of exercise consistent
with minimal exercise guidelines for persons with MS (Learmonth, 2023, p.1624).
While exercise interventions are generally considered safe for people with Multiple Sclerosis,
safety precautions and modifications may be required depending on the needs of the
individual. A 2019 systematic review of guidelines produced the following advice:
An exercise prescription for people with MS should promote a safe and individualized
exercise regimen. Thus, before prescribing an exercise routine, MS specific
symptoms/characteristics (i.e., fatigue and heat sensitivity) should be identified and
discussed, and the exercise prescription should include appropriate modifications. For
example, individuals with high heat sensitivity should exercise in a cool environment,
and a cooling fan should be readily available for the person during the exercise
sessions. When individuals experience symptom exacerbation, either daily variation in
symptoms or relapse, the exercise program may require modification or be temporarily
discontinued until the symptoms are stable. Risk of falling should be considered for
individuals with MS, and individuals with high risk of falls should perform both aerobic
and strength exercises in a seated position (e.g., recumbent bike, weight machines) and
under supervision (Kim et al, 2019, p.6)
Page 30 of 35
FOI 24/25-1212
7.3 Stage of progression
Learmonth et al (2023) did not find any significant difference in risk or safety of exercise
interventions between levels of disability. However, it should also be noted that participants
with advanced stages of MS were minimally represented in the studies reviewed. Of 40
randomised controlled trials, only 3 were focussed on people with severe symptoms of Multiple
Sclerosis. In fact, most evidence for the efficacy of exercise intervention for people with
Multiple Sclerosis lacks generalisability for people with severe symptoms (Corrini et al, 2023;
Taul-Madsen et al, 2021; Kim et al, 2019; Edwards & Pilutti, 2017).
Two systematic reviews have examined the effectiveness of physiotherapy or exercise
interventions in people with Multiple Sclerosis (Binshalan et al, 2022; Edwards & Pilutti, 2017).
A 2017 review found limited and very low certainty evidence that exercise interventions could
improve fitness, function, balance, fatigue, mood and quality of life (Edwards & Pilutti, 2017).
The authors also suggest exercise interventions are safe for people with severe symptoms.
More recently, Binshalan et al (2022) found low quality evidence that robot assisted gait
therapy may be effective at improving walking speed and endurance in people with severe
symptoms of Multiple Sclerosis. The authors speculate on possible reasons robot assisted gait
therapy may be more effective than other modes of physiotherapy or exercise intervention:
Appropriate PT intervention programs must be tailored to the patient’s abilities with
sufficient stimulus to push present competence to produce effect [49]. Therefore, it
possible that RAGT is less demanding for severely disabled pwMS, who might not be
able to complete other forms of PT effectively (p.13).
8. Muscular dystrophy
8.1 Frequency and duration
Hammer et al (2022) is the most recent systematic review of physiotherapy or exercise
interventions for people with muscular dystrophy. They reviewed 12 studies with 282
participants and found exercise intervention may improve strength and endurance for people
with MD. No conclusions regarding frequency, duration or intensity were possible with the
available evidence.
A 2019 Cochrane review of exercise training in muscle disease (including MD), notes:
The most effective dose of exercise for people with muscle diseases is currently
unknown, making it difficult to prescribe exercise in this population. This is reflected in
the large variation in the frequency, duration and intensity of exercise prescribed (Voet
et al, 2019, p.42).
Page 31 of 35
FOI 24/25-1212
8.2 Risks
The most recent review of physiotherapy or exercise interventions for MD noted that none of
the studies included in the review adequately reported on adverse events. However, the
authors noted that “intensive eccentric muscle exercise, where the muscle is both activated
and lengthened, in addition to high-resistance exercise, may exacerbate muscle damage and
should be avoided” (Hammer et al, 2022, p.2).
Voet et al (2019) report no evidence of safety concerns in appropriately structured exercise
programmes, though they also note that “included studies were small and the evidence was
largely low or low certainty; therefore, we can make no definitive statements regarding safety”
(p.42).
8.3 Stage of progression
No studies were able to discriminate benefits or risks of exercise based on severity of
symptoms or stage of progression.
9. References
Binshalan, T., Nair, K. P. S., & McNeil , A. (2022). The Effectiveness of Physiotherapy
Interventions for Mobility in Severe Multiple Sclerosis: A Systematic Review and Meta-
Analysis.
Multiple sclerosis international, 2022, 2357785.
https://doi.org/10.1155/2022/2357785
Baumann, A. N., Curtis, D. P., Chen, M., & Baldwin, K. D. (2023a). The Impact of the Addition
of a Physical Therapy Assistant to the Treatment Team for Management of Neck Pain:
A Retrospective Analysis of Outpatient Physical Therapy Clinics.
Cureus,
15(7),
e42751. https://doi.org/10.7759/cureus.42751
Baumann, A. N., Indermuhle, T., Oleson, C. J., Callaghan, M. E., Rogers, H., Pennacchio, C.,
Baldwin, K. D., & Leland, J. M., 3rd (2023b). Clinical Outcomes Associated With the
Addition of a Physical Therapist Assistant to a Rehabilitation Team When Treating
Musculoskeletal Shoulder Pain in the Outpatient Setting: A Retrospective Cohort Study.
Cureus,
15(7), e42680. https://doi.org/10.7759/cureus.42680
Corrini, C., Gervasoni, E., Perini, G., Cosentino, C., Putzolu, M., Montesano, A., Pelosin, E.,
Prosperini, L., & Cattaneo, D. (2023). Mobility and balance rehabilitation in multiple
sclerosis: A systematic review and dose-response meta-analysis.
Multiple sclerosis and
related disorders, 69, 104424. https://doi.org/10.1016/j.msard.2022.104424
Edwards, T., & Pilutti, L. A. (2017). The effect of exercise training in adults with multiple
sclerosis with severe mobility disability: A systematic review and future research
directions.
Multiple sclerosis and related disorders, 16, 31–39.
https://doi.org/10.1016/j.msard.2017.06.003
Page 32 of 35
FOI 24/25-1212
El Hayek, M., Lobo Jofili Lopes, J. L. M., LeLaurin, J. H., Gregory, M. E., Abi Nehme, A. M.,
McCall-Junkin, P., Au, K. L. K., Okun, M. S., & Sal oum, R. G. (2023). Type, Timing,
Frequency, and Durability of Outcome of Physical Therapy for Parkinson Disease: A
Systematic Review and Meta-Analysis.
JAMA network open,
6(7), e2324860.
https://doi.org/10.1001/jamanetworkopen.2023.24860
Ernst, M., Folkerts, A. K., Gol an, R., Lieker, E., Caro-Valenzuela, J., Adams, A., Cryns, N.,
Monsef, I., Dresen, A., Roheger, M., Eggers, C., Skoetz, N., & Kalbe, E. (2024).
Physical exercise for people with Parkinson's disease: a systematic review and network
meta-analysis.
The Cochrane database of systematic reviews,
4(4), CD013856.
https://doi.org/10.1002/14651858.CD013856.pub3
Grimes, D., Fitzpatrick, M., Gordon, J., Miyasaki, J., Fon, E. A., Schlossmacher, M.,
Suchowersky, O., Rajput, A., Lafontaine, A. L., Mestre, T., Appel-Cresswell, S., Kalia,
S. K., Schoffer, K., Zurowski, M., Postuma, R. B., Udow, S., Fox, S., Barbeau, P., &
Hutton, B. (2019). Canadian guideline for Parkinson disease.
CMAJ : Canadian Medical
Association journal = journal de l'Association medicale canadienne,
191(36), E989–
E1004. https://doi.org/10.1503/cmaj.181504
Hammer, S., Toussaint, M., Vol sæter, M., Nesbjørg Tvedt, M., Drange Røksund, O., Reychler,
G., Lund, H., & Andersen, T. (2022). Exercise Training in Duchenne Muscular
Dystrophy: A Systematic Review and Meta-Analysis.
Journal of rehabilitation medicine,
54, jrm00250. https://doi.org/10.2340/jrm.v53.985
Keus, S., Munneke, M., Graziano, M., Paltamaa, J., Pelosin, E., Domingos, J., ... & Bloem, B.
(2014).
European physiotherapy guideline for Parkinson’s disease. The Netherlands:
KNGF/ParkinsonNet.
Kim, Y., Lai, B., Mehta, T., Thirumalai, M., Padalabalanarayanan, S., Rimmer, J. H., & Motl, R.
W. (2019). Exercise Training Guidelines for Multiple Sclerosis, Stroke, and Parkinson
Disease: Rapid Review and Synthesis.
American journal of physical medicine &
rehabilitation,
98(7), 613–621. https://doi.org/10.1097/PHM.0000000000001174
Kyriakatis, G. M., Lykou, P. M., Dimitriadis, Z., & Besios, T. (2023). Efficacy of remote exercise
and physiotherapy programs on depressive symptoms in people with multiple sclerosis -
A systematic review and meta-analysis.
Multiple sclerosis and related disorders, 79,
105067. https://doi.org/10.1016/j.msard.2023.105067
Lau, B., March, M. K., Harmer, A. R., Caruana, S., Mahony, C., & Dennis, S. (2024).
Experiences of Boosting Inpatient Exercise After HipFracture Surgery Using An
Alternative Workforce - A Qualitative Study.
BMC geriatrics,
24(1), 183.
https://doi.org/10.1186/s12877-024-04756-1
Learmonth, Y. C., P Herring, M., Russel , D. I., Pilutti, L. A., Day, S., Marck, C. H., Chan, B.,
Metse, A. P., & Motl, R. W. (2023). Safety of exercise training in multiple sclerosis: An
updated systematic review and meta-analysis.
Multiple sclerosis (Houndmil s,
Page 33 of 35
FOI 24/25-1212
Basingstoke, England),
29(13), 1604–1631.
https://doi.org/10.1177/13524585231204459
Meng, L., Li, X., Li, C., Tsang, R. C., Chen, Y., Ge, Y., & Gao, Q. (2020). Effects of exercise in
patients with amyotrophic lateral sclerosis: a systematic review and meta-analysis.
American Journal of Physical Medicine & Rehabilitation,
99(9), 801-810.
https://doi.org/10.1097/PHM.0000000000001419
Motor Neuron Disease Australia. (2021).
Physical Activity and MND.
https://www.mndaustralia.org.au/mnd-connect/information-resources/physical-activity-
and-mnd
National Institute of Health and Care Excellence. (2017).
Parkinson’s disease in adults:
diagnosis and management [NG71]. https://www.nice.org.uk/guidance/ng71
O’Callaghan, G., Murray, D. & Vance, R. (2014). Guidelines for the physiotherapy
management of Motor Neuron Disease. Irish Hospice Foundation.
https://d2khofxhx95v1k.cloudfront.net/b1fdb917f1fea268a7a1b7b502dcd172.pdf
Osborne, J. A., Botkin, R., Colon-Semenza, C., DeAngelis, T. R., Gallardo, O. G., Kosakowski,
H., Martel o, J., Pradhan, S., Rafferty, M., Readinger, J. L., Whitt, A. L., & El is, T. D.
(2022). Physical Therapist Management of Parkinson Disease: A Clinical Practice
Guideline From the American Physical Therapy Association.
Physical therapy,
102(4),
pzab302. https://doi.org/10.1093/ptj/pzab302
Papadopoulou, M., Papapostolou, A., Dimakopoulos, R., Salakou, S., Koropouli, E.,
Fanouraki, S., Bakola, E., Moschovos, C., & Tsivgoulis, G. (2024). Non-
Pharmacological Interventions on Pain in Amyotrophic Lateral Sclerosis Patients: A
Systematic Review and Meta-Analysis.
Healthcare (Basel, Switzerland),
12(7), 770.
https://doi.org/10.3390/healthcare12070770
Sarigiovannis, P., Foster, N. E., Jowett, S., & Saunders, B. (2023). Developing a best practice
framework for musculoskeletal outpatient physiotherapy delegation: the MOPeD mixed-
methods research study protocol.
BMJ open,
13(3), e072989.
https://doi.org/10.1136/bmjopen-2023-072989
Sarigiovannis, P., Foster, N. E., Jowett, S., & Saunders, B. (2022). Delegation of workload
from musculoskeletal physiotherapists to physiotherapy assistants/support workers: A
UK online survey.
Musculoskeletal science & practice, 62, 102631.
https://doi.org/10.1016/j.msksp.2022.102631
Sarigiovannis, P., Jowett, S., Saunders, B., Corp, N., & Bishop, A. (2021). Delegation by Al ied
Health Professionals to Al ied Health Assistants: a mixed methods systematic review.
Physiotherapy, 112, 16–30. https://doi.org/10.1016/j.physio.2020.10.002
Snowdon, D. A., Wang, Y. T., Cal isaya, M. L., Col yer, T. A., Jol iffe, L., Johns, N., Vincent, P.,
Pragash, N., & Taylor, N. F. (2024). Staying Active with Multimorbidity In Acute hospital
settings (StAMInA) trial: protocol for a feasibility randomised controlled trial of al ied
Page 34 of 35
FOI 24/25-1212
health assistant mobility rehabilitation for patients with multimorbidity.
BMJ open,
14(1),
e078843. https://doi.org/10.1136/bmjopen-2023-078843
Snowdon, D. A., King, O. A., Dennett, A., Pinson, J. A., Shannon, M. M., Collyer, T. A., Davis,
A., & Wil iams, C. M. (2022). Delegation of patient related tasks to allied health
assistants: a time motion study.
BMC health services research,
22(1), 1280.
https://doi.org/10.1186/s12913-022-08642-7
Snowdon, D. A., Vincent, P., Cal isaya, M. L., Col yer, T. A., Wang, Y. T., & Taylor, N. F.
(2021). Feasibility of allied health assistant management of people with acute hip
fracture: protocol for a feasibility randomised controlled trial.
BMJ open,
11(11),
e054298. https://doi.org/10.1136/bmjopen-2021-054298
Snowdon, D. A., Storr, B., Davis, A., Taylor, N. F., & Wil iams, C. M. (2020). The effect of
delegation of therapy to allied health assistants on patient and organisational outcomes:
a systematic review and meta-analysis.
BMC health services research,
20(1), 491.
https://doi.org/10.1186/s12913-020-05312-4
Taul-Madsen, L., Connolly, L., Dennett, R., Freeman, J., Dalgas, U., & Hvid, L. G. (2021). Is
Aerobic or Resistance Training the Most Effective Exercise Modality for Improving
Lower Extremity Physical Function and Perceived Fatigue in People With Multiple
Sclerosis? A Systematic Review and Meta-analysis.
Archives of physical medicine and
rehabilitation,
102(10), 2032–2048. https://doi.org/10.1016/j.apmr.2021.03.026
Voet, N. B., van der Kooi, E. L., van Engelen, B. G., & Geurts, A. C. (2019). Strength training
and aerobic exercise training for muscle disease.
The Cochrane database of systematic
reviews,
12(12), CD003907. https://doi.org/10.1002/14651858.CD003907.pub5
Zhou, B., Wei, J., Zhang, Y., Liu, Y., Shan, S., Ye, S., Li, B., Fan, D., & Luo, Y. (2022).
Different observation period of exercise training in amyotrophic lateral sclerosis
patients: A meta-analysis.
Frontiers in neurology, 13, 986882.
https://doi.org/10.3389/fneur.2022.986882
Page 35 of 35